After four years of fighting about it, the World Health Organization has finally proclaimed that viruses, including the SARS-CoV-2 virus that causes COVID, can be spread through the air.
The operative phrase here is “through the air.” It’s plain language that anyone can understand, and this switch from jargon such as “airborne” and “aerosol” may finally clear the way for researchers to get funding to study better, real-life ways to protect people from a range of infectious diseases.
And just maybe governments, retailers, school authorities and others can now start to get solid information about ways they can clean indoor air. While it is going to take more than a wordy WHO statement to persuade gym owners that fogged-up windows mean too many people are huffing out potentially infectious air, the new wording does provide a better explanation of why it’s gross and unhealthy.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
It took four years to get here because some leaders in public health, medicine and science clung too tightly to precision and semantics. No one disputes that respiratory viruses are spread by droplets. The disagreements were over what sized droplets really counted as droplets, whether they hung in the air and how far they traveled. There were debates over the definition of “aerosol” and what sized droplet that meant. Some experts refused to say—or to let anyone else say—that a droplet could remain suspended in air or travel over a distance unless it was, technically, an aerosol. They said that meant it had to be five microns or less in size—a definition that itself did not have a basis in modern science.
One particular moment of shame came on March 28, 2020, when WHO tweeted: “FACT: #COVID19 is NOT airborne.”
So the initial guidance for people was that the virus was carried in droplets that fell to surfaces. It is transported that way, as are other viruses, and cleaning and disinfecting surfaces is useful in fighting a range of microbes.
But it’s not the only way they spread. In the battle over what “aerosol” and “airborne” meant, public health officials lost sight of what was right in front of them: people were catching COVID by breathing contaminated air.
“It’s terrible that it took them years,” José-Luis Jiménez, a chemistry professor and aerosol expert at the University of Colorado, said. “By the end of March 2020, a lot of scientists had contacted them. It’s not like they didn’t have access to the information,” added Jiménez, who has detailed the history of mainstream public health resistance to the idea of airborne spread.
WHO and other agencies such as the Centers for Disease Control and Prevention did come around eventually, and it’s now broadly agreed that, along with measles, smallpox and tuberculosis, other infectious diseases can linger in the air and spread across rooms. “The descriptor ‘through the air’ can be used in a general way to characterize an infectious disease where the main mode of transmission involves the pathogen travelling through or being suspended in the air,” WHO now says.
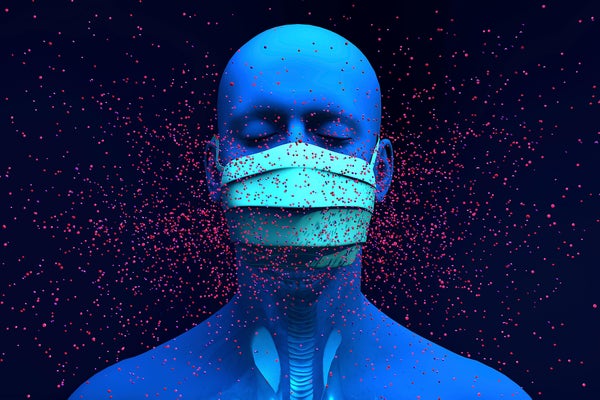
The agency also states: “These potentially infectious particles are carried by expired airflow, exit the infectious person’s mouth/nose through breathing, talking, singing, spitting, coughing or sneezing and enter the surrounding air. From this point, these particles are known as ‘infectious respiratory particles’ or IRPs.” There’s no definition of particle size and no cutoff for when these germy expectorations will end with a splat on the floor instead of making their way into someone else’s eyes, nose or mouth.
This should clear the way for funding more and better research on the transmission of infectious diseases—not just COVID, but influenza, respiratory syncytial virus (RSV) and viruses that cause the common cold. That, in turn, should give managers of schools, retailers, airports and other public spaces the information they need to help keep air and surfacers cleaner. Because if people understand the physics of disease transmission, they can find ways to safely keep schools, shops and restaurants open during outbreaks and epidemics with better practices in ventilation, air and surface cleaning and foot traffic control.
Cases of influenza, RSV and other respiratory infections plummeted during the height of the COVID pandemic. Researchers are still studying why, but closures of schools and restaurants, remote working, handwashing, distancing and mask use all played strong roles. Flu, RSV and other respiratory infections came roaring back in 2024 as people returned to offices, schools, restaurants and large gatherings, largely without masks.
Could restaurants with ultraviolet lights and fans in the ceilings offer safer spaces to eat out during flu season? Can schools stay open even during disease outbreaks with upgrades to HVAC systems and low-tech fixes like windows that actually open? Ananya Iyengar of the Johns Hopkins Center for Health Security and colleagues took a look at how one New York school kept infections down during the pandemic, for example, and found better ventilation improved indoor air quality. The cost? Along with a suite of other measures, about $880 per student per year.
Words matter. When people heard that COVID might spread on surfaces, they wasted time wiping down groceries. People who misunderstood airborne spread needlessly wore masks on outdoor walks and veered off sidewalks to avoid their neighbors. Stores spent countless dollars and employee-hours pasting “keep six feet apart” signs on the floor and routing one-way traffic through aisles in what was almost certainly a futile effort to limit disease spread.
Instead, an understanding of how viruses can drift out of an infected person’s nose or mouth and then transmit infections for more than four hours can encourage a teacher to air out a classroom in between classes or a bar owner to serve drinks on the patio instead of forcing customers to jam together inside.
Another potential benefit: clearing air of germs will also cleanse it of pollen, spores and other particles that cause allergies and worsen asthma. Better circulation can also help clear out potentially toxic chemical fumes and dust. Residents of Louisiana still remember the noxious formaldehyde found polluting trailers FEMA supplied to Hurricane Katrina survivors. Better ventilation standards for new homes could reassure homeowners that they are not only at less risk for catching something nasty from their school-aged children, but also potentially safer from off-gassing carpets and furniture or mold spores. If people had cleaner indoor air all year long, would that cut annual cases of flu, the common cold and even asthma and allergies?
There’s no guarantee a future administration won’t once again mix up the messaging, but there will be much less excuse for government officials telling Americans they do not need to wear masks, as then surgeon general Jerome Adams did in a February 2020 post on Twitter. It will take years if not decades to win back the trust lost by the conflicting advice, but at least now some understandable language is available to use.
The new federal health research agency, the Advanced Research Projects Agency for Health or ARPA-H, has launched an effort called BREATHE, short for Building Resilient Environments for Air and Total HEalth, that promises to fund studies aimed at improving indoor air in buildings. The agency is asking for ideas and bids for ways to clean up indoor air in the same way water treatment and sewer systems revolutionized public health a century ago. It’s a worthwhile area of study that deserves adequate funding.
“It’s now respectable to do this research,” Jiménez said. “People can get funding to do some research about indoor air and engineering systems. They are stepping into fields that they really wouldn’t work on before. So you see some encouraging changes.”
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.